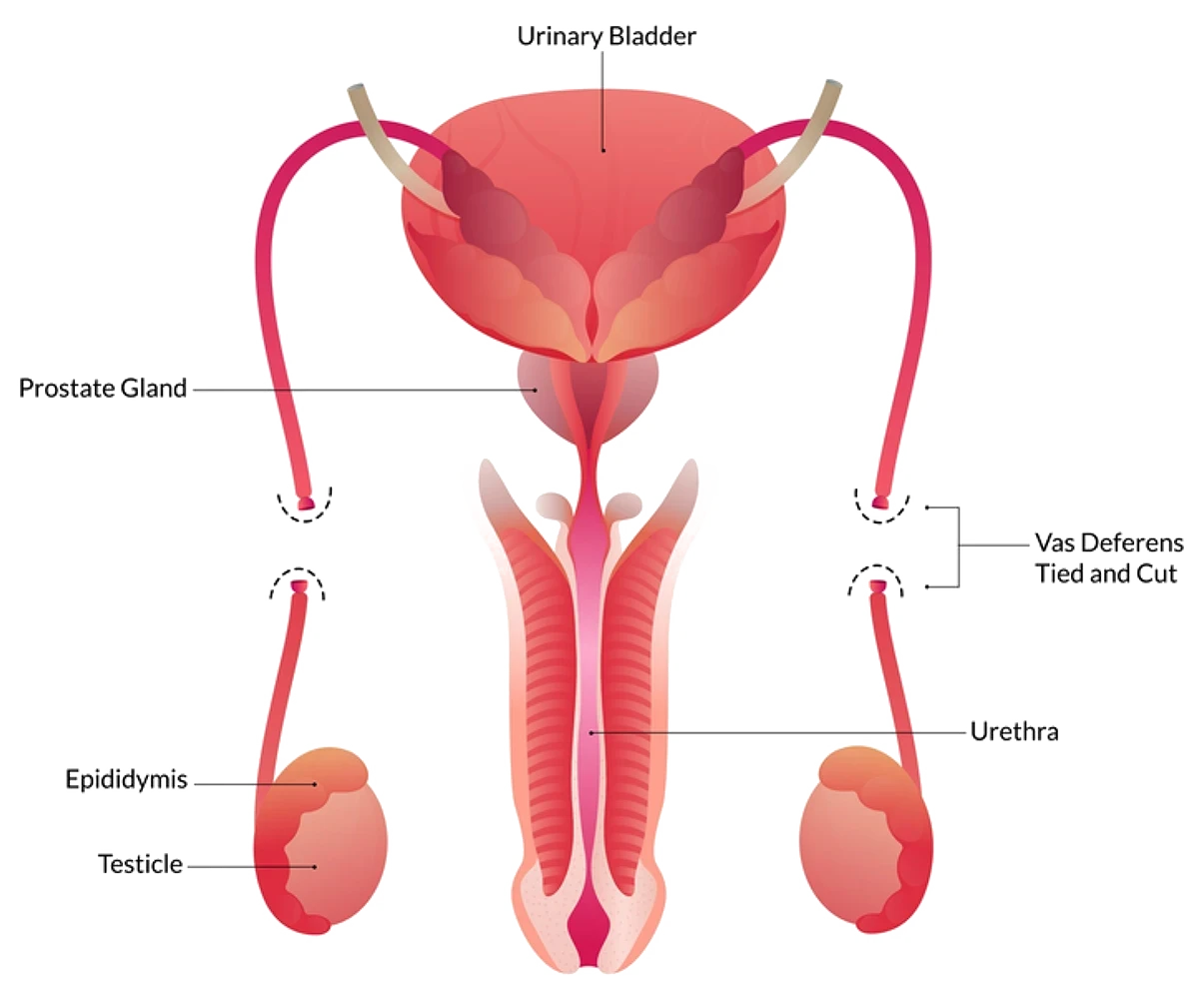
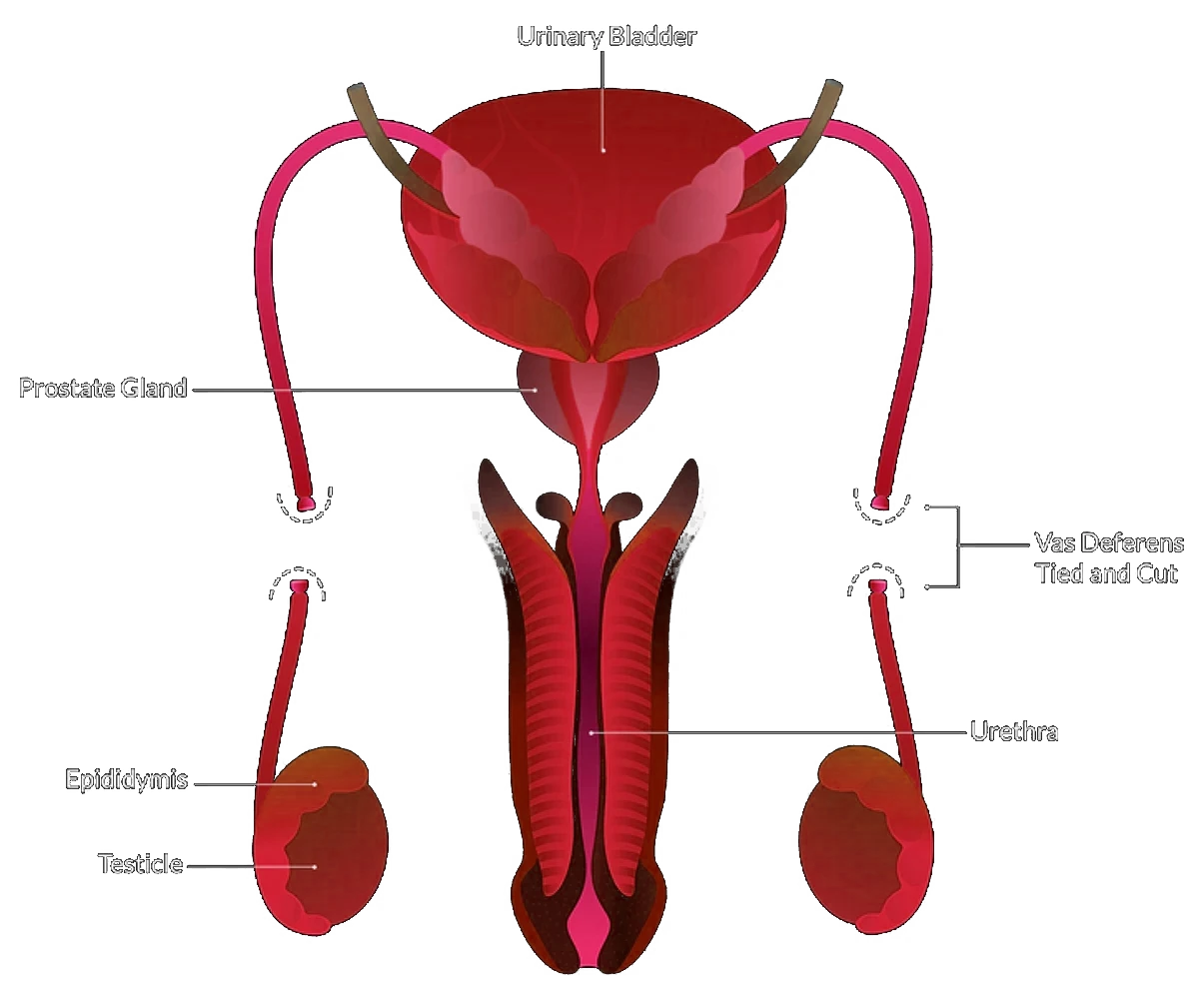
A vasectomy is a surgical procedure that involves cutting or blocking the vas deferens, the tubes that transport sperm from the testicles to the prostate. This prevents sperm from mixing with semen, thereby rendering the man sterile (unable to father children). The volume and appearance of semen remain unchanged after the procedure.
Male anatomy and vasectomy
In the male reproductive system:
- The testes produce sperm.
- Sperm travel via the vas deferens to the prostate, where they combine with seminal fluid.
A vasectomy interrupts this pathway by blocking or severing the vas deferens, so sperm no longer enter the semen.
Why consider a vasectomy?
Vasectomy is a highly effective and permanent form of contraception. Its benefits include:
- Greater reliability than condoms, withdrawal, contraceptive pills, or other temporary methods
- A safer, simpler, and more cost-effective option compared to female sterilisation (tubal ligation)
Who is a candidate?
Vasectomy is typically suited for men who:
- Are certain that they no longer wish to have children
- Wish to seek a more permanent form of contraception
Important: Men under the age of 25 should carefully consider the decision to have such a procedure. If you
have any doubts surrounding your circumstances changing in the future, you should not have the procedure.
Addressing concerns - vasectomy and masculinity
Concerns about masculinity or sexual performance post-vasectomy are not supported by medical evidence. Specifically:
- Testosterone production and secondary sexual traits (e.g. beard growth, voice depth) remain unaffected
- Sexual drive, erections, and orgasms are preserved
- Only a small portion of ejaculate consists of sperm, so semen appearance and volume remain virtually unchanged
Vasectomy and fertility
Sterility is not immediate after the procedure. Sperm may still be present in the vas deferens beyond the surgical site. It usually takes 10 to 15 ejaculations to clear residual sperm. Sterility is confirmed through a follow-up semen analysis.
Protection against STDs
A vasectomy does not protect against sexually transmitted diseases (STDs), including HIV/AIDS. Condoms should still be used when there is any risk of STI transmission or acquisition.
Before your vasectomy
Prof Lawrentschuk needs your full medical history to plan the procedure safely. If you have not already done so, please inform him about:
- Allergies to medications, anesthesia, or surgical tapes.
- Issues with prolonged bleeding or excessive bruising.
- Previous surgeries involving the testicles or hernia repair.
- Current or past illnesses, including psychological conditions.
Also, please let Prof Lawrentschuk know if your list of medications has changed. This includes aspirin,
medicines containing aspirin (such as cough syrups), Palvix, warfarin, anti-inflammatory medications (such
as Nurofen), vitamin E, herbal medications, fish oil or garlic tablets. Certain medications can increase the risk
of bleeding, so Prof Lawrentschuk may recommend adjustments.
Anaesthetic options
Your vasectomy can be performed under:
- Local anesthesia: Numbs the surgical area while you remain awake.
- General anesthesia: You are asleep for the procedure.
Modern anesthesia is generally safe, though complications are possible. Prof Lawrentschuk will discuss any
risks with you
Surgical methods
The procedure typically takes 15 to 30 minutes. Prof Lawrentschuk will recommend one of the following methods based on your preferences and medical considerations:
Conventional Approach
A small scrotal incision is made; the vas deferens is cut, sealed, and the site stitched closed.
No-scalpel Approach
Instead of an incision, a puncture technique is used to provide access to the vas deferens, often without stitches.
Open-End Vasectomy
The testicular end of the vas deferens is left open to reduce pressure and potential discomfort.
Recovery after surgery
Recovery is generally smooth, with minor discomfort. You may experience some swelling, bruising, and a dull ache. These symptoms can be minimised by wearing supportive underwear and applying ice packs.
- Incision Care: Use gauze pads as needed and follow Prof Lawrentschuk’s instructions regarding bathing and showering.
- Pain Relief: Over-the-counter painkillers like paracetamol are usually sufficient.
- Activity: Avoid strenuous activity for at least two weeks. Gradually resume sports and physical labour once discomfort subsides.
- Sexual Activity: You can resume sex when you feel comfortable, but continue using contraception until Prof Lawrentschuk confirms sterility.
Possible complications
While vasectomy is generally safe, complications can occur. These may include:
Infection
It can occur at the surgical site and in the nearby tissues. The site may appear red, swollen and tender. If you
experience this, please contact Prof Lawrentschuk’s rooms, your local GP or visit your closest Emergency
Department.
Swelling and bruising
Blood or fluid may accumulate in the skin of the scrotum, causing swelling and bruising. The body will
reabsorb small amounts of fluid but larger amounts may need to be drained by Prof Lawrentschuk. This rarely
requires extra surgery.
Small, tender and painful lumps
Sperm can occasionally leak from the cut ends of the vans deferens into the surrounding tissue. This can lead
to small bumps forming under the skin of the scrotum. Often, no treatment is needed; some people take anti-
inflammatory medication to ease any pain.
Chronic pain
Although rare, some men experience consistent discomfort in the scrotum and others feel pain only during
sex. If you experience this, anti-inflammatory drugs can help to ease discomfort. If it is still persistent, please
book in to see Prof Lawrentschuk as it may be in your best interest to reverse the procedure.
Spontaneous reconnection of the vas deferens
The cut ends of the vans deferens may rejoin months or years following the procedure. This can even occur
after a completely negative sperm count.
Follow-up and monitoring
You will usually have a follow-up appointment with Prof Lawrentschuk or our Urology Nurse, Thili, 3 months following your procedure. In preparation for this appointment, you will be issued a semen analysis pathology request slip. Please ensure this is completed 1-2 weeks prior to your scheduled appointment and that you have had at least 20 ejaculations between your procedure and this test.
Please note that there are only select pathology collection sites available for semen analysis. If you are unsure about where to go, please email our rooms and we can provide you with some locations.
If you have any queries, please use the contact details below:
MONDAY to FRDAY 8:30AM–4:00PM
Call the rooms at 9329 1197
AFTER HOURS
Contact Epworth Emergency on 03 9426 6666 or Royal Melbourne Emergency on 03 9342 7000.
You can also page Prof Lawrentschuk on 03 9387 1000.
For appointments and enquiries:
CONSULTING LOCATIONS