A hydrocoele repair is a surgical procedure to remove a hydrocoele which is a fluid-filled sac that develops around the testicle. While hydrocoeles are usually harmless, they can become uncomfortable or interfere with daily activities. This procedure is considered when the hydrocoele causes pain, swelling, or significant inconvenience.
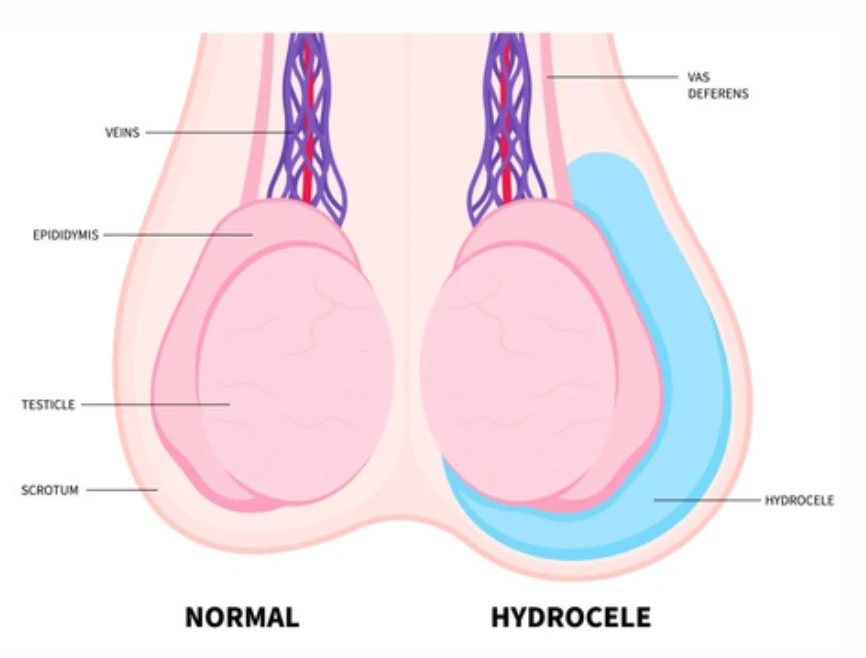
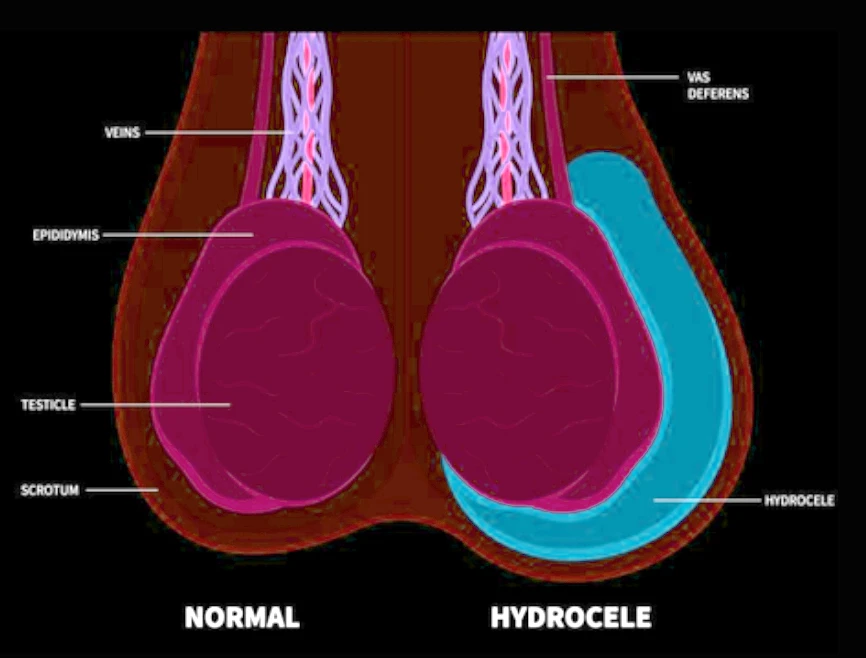
What is a hydrocoele?
A hydrocoele is a fluid collection within the sac surrounding the testicle, known as the tunica vaginalis. This fluid is normally produced by the lining membrane, but in some cases it can accumulate excessively, forming a hydrocoele.
Hydrocoeles are common and typically benign. In most cases, there is no identifiable cause. However, hydrocoeles may occasionally be linked to:
- Scrotal infections (e.g. epididymitis)
- Trauma to the scrotum
- Previous scrotal surgery
- Testicular cancer
Why is surgery recommended?
A hydrocoelectomy (surgical removal of the hydrocoele) is not always necessary. However, Prof Lawrentschuk may recommended it if:
- The hydrocoele causes pain
- It interferes with daily activities or quality of life
What does the procedure involve?
Hydrocoelectomy is typically performed under general anaesthetic, although spinal anaesthesia (numbness from the waist down) is also an option. Prof Lawrentschuk will help guide you to which option is best for you.
- A small incision is made in the scrotum.
- The fluid is drained, and the sac surrounding the testicle is partially removed.
- The incision is closed with dissolvable stitches.
- In some cases, a temporary plastic drain is inserted and removed within 1–2 days.
The procedure is usually completed as day surgery. Patients can often return home the same day, provided they are accompanied by a responsible adult. Occasionally, an overnight hospital stay is required.
Before surgery
You will be contacted 1–2 weeks prior to your scheduled procedure with specific fasting instructions and hospital admission details. You will also receive a link to complete your online admission forms.
It is important to advise the rooms if you are taking any blood thinners or any prescribed medications for diabetes or weight loss purposes. The rooms can be contacted on 9329 1197
Following surgery
Recovering at home
Once discharged, please note the following:
- Rest for the first 1–2 days after surgery is advised.
- Supportive underwear (e.g. jockstrap, speedos, or two pairs of tight briefs) should be worn for at least one week.
- Return to sedentary work is typically possible after 4–7 days.
- Gentle exercise may resume after approximately one week.
- Avoid strenuous exercise, cycling, or heavy lifting for at least four weeks.
- Swimming should be avoided for two weeks.
- Driving can generally resume after 2–5 days, once safe control (e.g. emergency braking) is possible.
- Sexual activity may resume when comfortable, usually after two weeks.
- This procedure does not affect testosterone levels, sperm production, or erectile function.
Are there any alternatives?
The following alternative methods for hydrocoele repair are listed below:
- Observation (no treatment): Appropriate if the hydrocoele is not causing discomfort or issues.
- Aspiration: Involves removing fluid with a needle. However, fluid typically reaccumulates within weeks.
If you are uncertain whether surgery is the best option, please speak to Prof Lawrentschuk to discuss what is most appropriate for your situation.
Possible complications
Common (1 in 2 to 1 in 10):
- Swelling and discomfort in the scrotum for weeks to months post-operatively
- Temporary reaccumulation of fluid in the scrotum
- Long-term firmness or irregularity of the testicle
Occasional (1 in 10 to 1 in 50):
- Recurrence of the hydrocoele
Rare (1 in 50 to 1 in 250):
- Bleeding in the scrotum requiring further surgery
- Infection requiring antibiotics or additional procedures
- Wound breakdown or delayed healing
- Urinary retention necessitating catheter insertion
Very rare (<1 in 250):
- Injury to the testicle, epididymis, or spermatic cord, potentially requiring testicle removal
- Chronic scrotal pain
When to seek help
Please contact Professor Lawrentschuk’s rooms at 9329 1197 or attend your nearest Emergency Department if you experience:
- Excessive pain that doesn’t ease with medication.
- A fever over 38.5°C.
- Bright red blood coming from the scrotum.
- Excessive redness, swelling, or warmth in the scrotum.
Follow-up and monitoring
You will usually have a follow-up appointment with Prof Lawrentschuk within 6-8 weeks after surgery to assess your recovery and evaluate the next steps needed.
If you have any queries, please use the contact details below:
MONDAY to FRDAY 8:30AM–4:00PM
Call the rooms at 9329 1197
AFTER HOURS
Contact Epworth Emergency on 03 9426 6666 or Royal Melbourne Emergency on 03 9342 7000.
You can also page Prof Lawrentschuk on 03 9387 1000.
For appointments and enquiries:
CONSULTING LOCATIONS