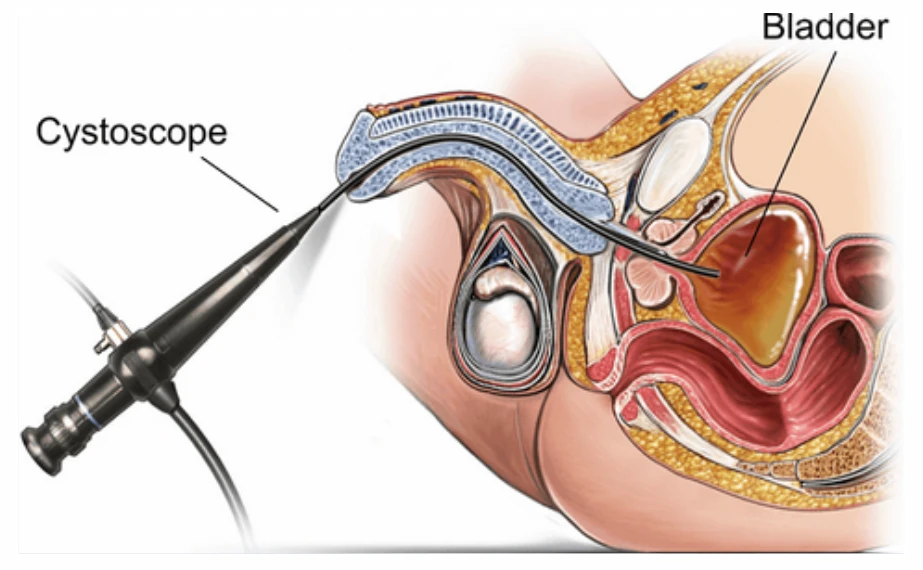
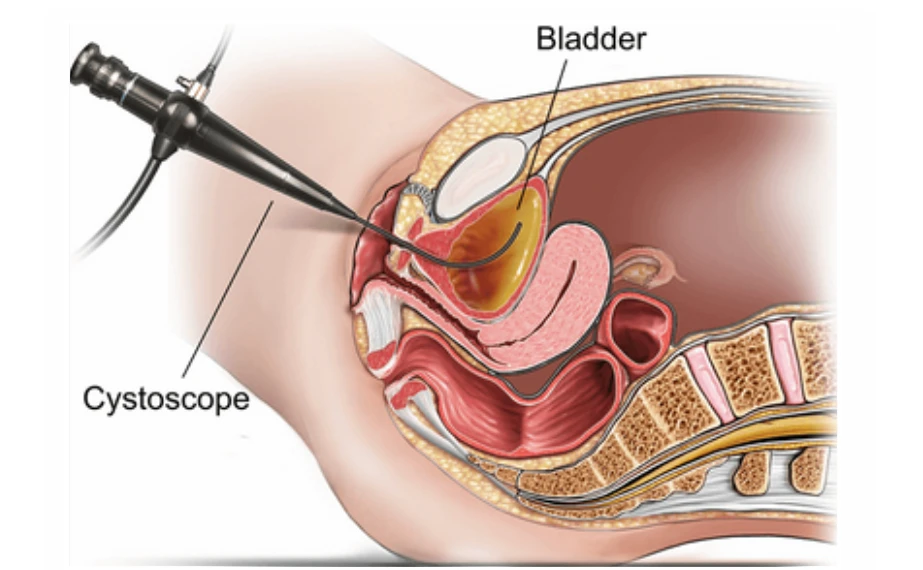
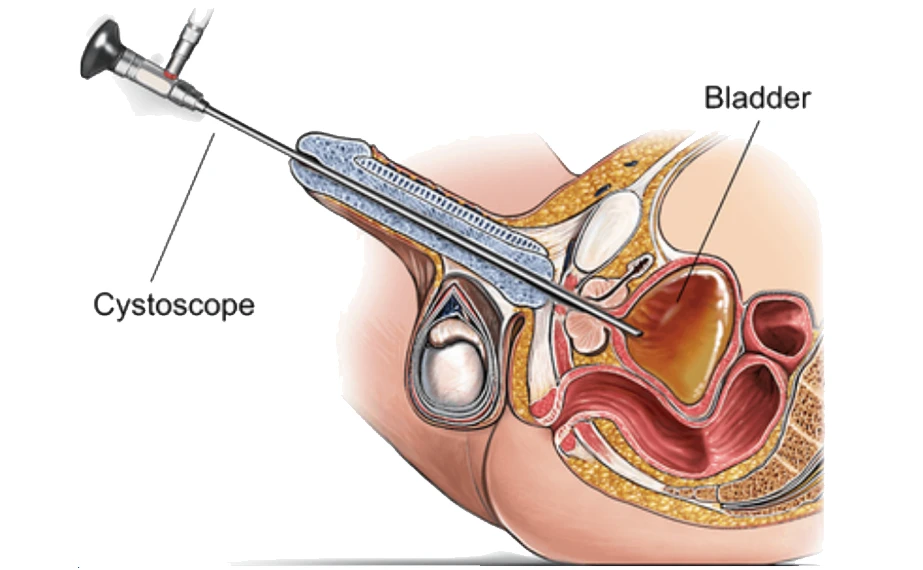
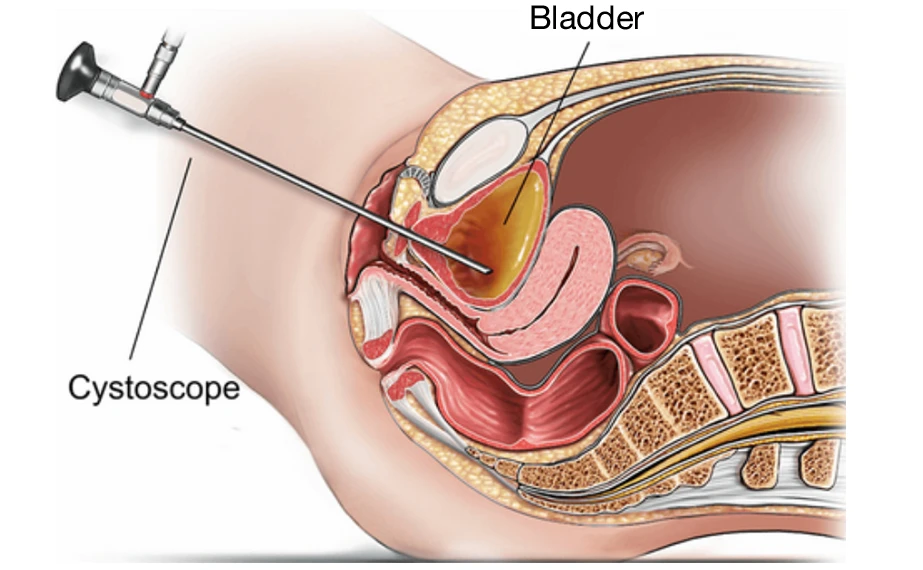
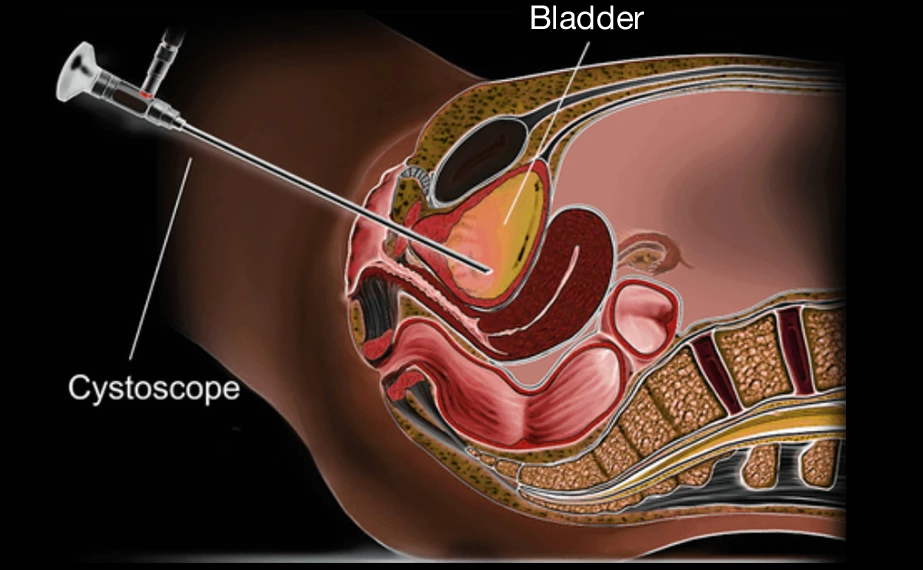
A cystoscopy is a procedure that allows Prof Lawrentschuk to visually examine the inside of your bladder and urethra using a thin telescope known as a cystoscope. The scope is passed through the urethra (the tube you pass urine through) and into the bladder.
Why is a cystoscopy required?
Cystoscopy is used to investigate a variety of urinary symptoms and conditions. Common reasons include:
- Blood in the urine
- Recurrent urinary tract infections
- Urinary issues such as frequency, urgency, incontinence, or difficulty emptying the bladder
- Surveillance for bladder cancer recurrence
Cystoscopy can also be used during other procedures, such as:
- Evaluation of abnormalities in the bladder wall (e.g. biopsies)
- Removal of ureteric stents
Types of cystoscopies and what to expect
The two main types of cystoscopies performed by Prof Lawrentschuk include the flexible cystoscopy and the rigid cystoscopy. Information on both types can be found below.
Flexible Cystoscopy
A flexible cystoscopy is often performed while you are awake or with light sedation. It is a quick procedure.
- The genital area is cleaned and a lubricating jelly is applied into the urethra.
- A thin, flexible scope is gently passed through the urethra into the bladder.
- The bladder is filled with sterile water to allow for full inspection.
- Once the bladder is examined, the scope is removed and you may empty your bladder.
These are usually completed as day procedures, meaning you may go home the same day.
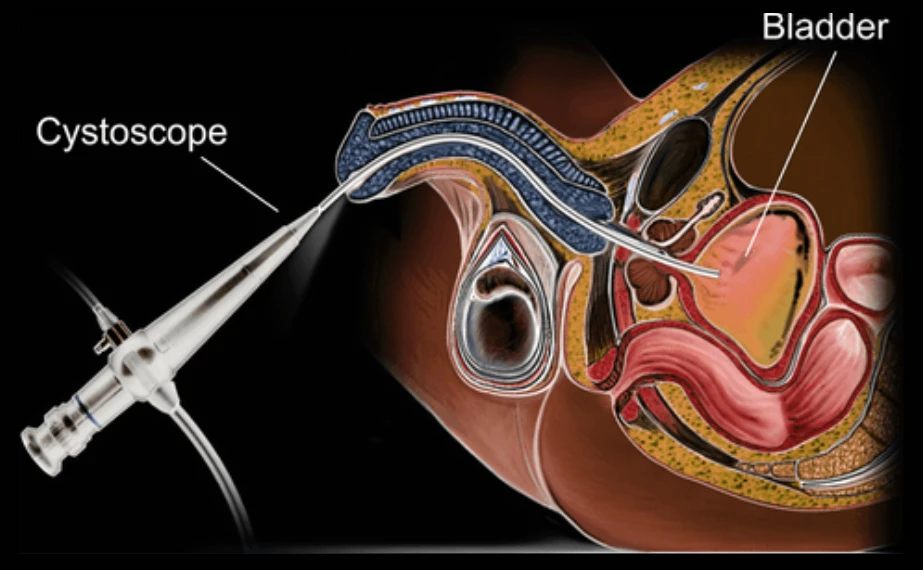
Rigid cystoscopy in males
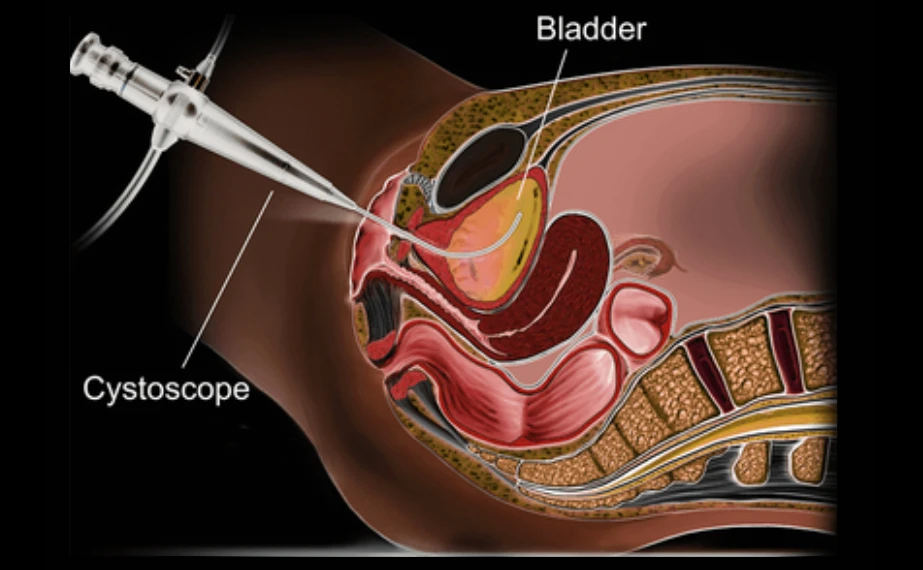
Rigid cystoscopy in females
Rigid Cystoscopy
A rigid cystoscopy is performed in hospital under general or spinal anaesthetic.
- A rigid (non-flexible) scope is passed through the urethra into the bladder.
- The bladder is filled with sterile water for optimal visualisation.
Prof Lawrentschuk commonly uses a rigid cystoscope when performing the following:
- Biopsy of bladder tissue
- Dilatation of urethral strictures
- Cauterisation of bleeding areas
- Removal of ureteric stents or foreign bodies
- Botox injections into the bladder
Following the procedure, a catheter may be inserted temporarily. Most patients are discharged the same day, though overnight stay may be required if a catheter is placed.
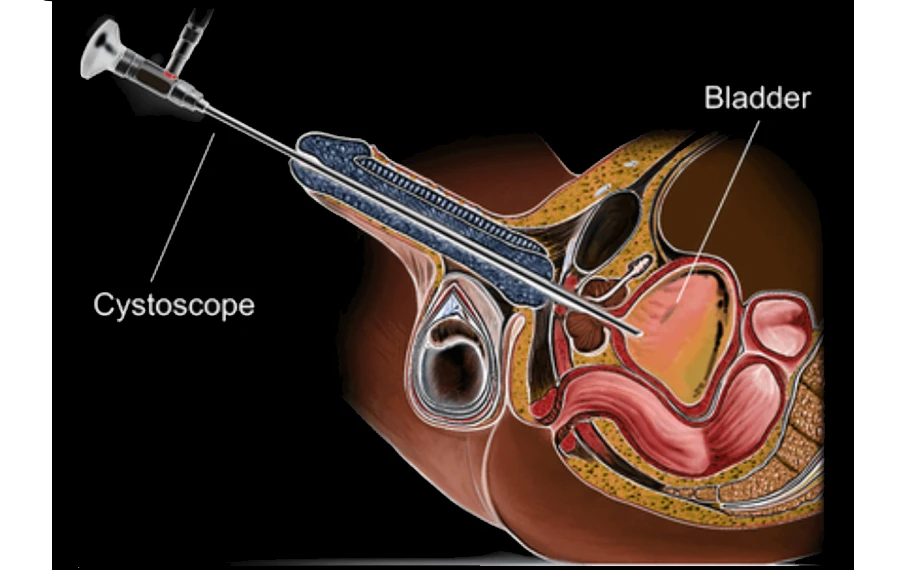
Fleixble cystoscopy in males
Fleixble cystoscopy in females
Are there any alternatives?
Imaging (such as ultrasound or CT scans) and urine tests can sometimes be used to investigate urinary problems. However, these alternatives are often less reliable than direct visual inspection with cystoscopy.
Before your procedure
You will be contacted 1–2 weeks prior to your scheduled procedure with specific fasting instructions and hospital admission details. You will also receive a link to complete your online admission forms.
It is important to advise the rooms if you are taking any blood thinners or any prescribed medications for diabetes or weight loss purposes. The rooms can be contacted on 9329 1197
Following your procedure
Recovering at home
Once discharged, please note the following:
- Mild burning or stinging with urination and light bleeding are common for 1–2 days.
- If you had a flexible cystoscopy while awake, you can usually resume work the same day.
- If you had sedation or anaesthetic, allow 1–2 days before returning to work and avoid driving for 24 hours.
Possible complications
Occasional (1 in 10 to 1 in 50):
- Urinary tract infection (may require antibiotics)
Rare (1 in 50 to 1 in 250):
- Bleeding that requires further treatment
- Urethral injury leading to scarring
Very rare (< 1 in 250):
- Injury to the bladder wall requiring surgical repair
When to seek help
Please contact Professor Lawrentschuk’s rooms at 9329 1197 or attend your nearest Emergency Department if you experience:
- Inability to urinate.
- Excessive pain that you can’t control with your prescribed medications or simple pain relief medications.
- Large clots in the urine.
- A fever.
Follow-up and monitoring
Depending on the findings of your cystoscopy, Prof Lawrentschuk will advise the team of what follow-up he you to be scheduled in for. We will contact you to book this in and find a time that best suits your would like schedule.
If you have any queries, please use the contact details below:
MONDAY to FRDAY 8:30AM–4:00PM
Call the rooms at 9329 1197
AFTER HOURS
Contact Epworth Emergency on 03 9426 6666 or Royal Melbourne Emergency on 03 9342 7000.
You can also page Prof Lawrentschuk on 03 9387 1000.
For appointments and enquiries:
CONSULTING LOCATIONS